Excretory system
Excretion or waste elimination is carried out by four organ systems:
|
Organ System
|
Organ
|
Waste material
|
|
Respiratory system
Integumentary system
Digestive system
Urinary system
|
Lungs
Skin
Liver
Large intestine
Kidneys
|
CO2, small amounts of other gases, H2O
H2O, inorganic salts, lactic acid, urea
Not only eliminate food residue but also actively excretes H2O, salts, CO2, lipids, bile pigments, cholesterol, etc.
Broad variety of metabolic wastes, toxins, drugs, hormones, salts, H+, H2O
|
However, the primary organs for waste elimination are the kidneys. The kidneys in general are also capable of performing the following functions:
· Filters blood plasma, separate wastes from the useful chemicals and eliminate the wastes while returning the rest to the blood stream;
· Regulate blood volume and pressure by eliminating or conserving water as necessary;
· Regulate the osmolarity of the body fluids by controlling the relative amounts of water and solutes eliminated;
· Secrete the enzyme renin, which activates hormonal mechanisms that control blood pressure and electrolyte balance;
· Secrete the hormone erythropoietin, which controls the RBC count and oxygen-carrying capacity of blood
· Function with the lungs to regulate the PCO2 and acid-base balance of body fluids
· Control homeostasis through their role in synthesizing calcitriol
· Detoxify superoxides, free radicals and drugs with the use of peroxisomes
· In times of starvation, they deaminate amino acids
Urinary System
Composed of kidneys, ureters, urinary bladder, urethra
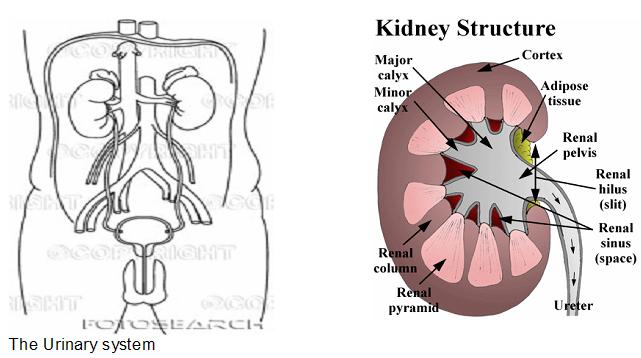
1. Kidneys: paired reddish-brown, bean-shaped organs on posterior abdominal wall; retroperitoneal
n Tissue layer surrounding the kidneys: three layers: (1) renal capsule (fibrous), (2) adipose capsule (perirenal fat) (3) renal fascia (double-layered)
- External structure of the kidney:
Renal hilus – medial indentation; passageway for blood vessels and ureters
Renal pelvis located in renal sinus
n Internal structure of the kidney:
Cortex – outer layer; also forms renal columns that pass into medulla
Medulla – consists of renal pyramids
Renal pelvis – expanded upper end of ureter; formed from joining of major calyces
n Renal tubules: functional units of kidneys; consists of nephrons and collecting tubules. Each nephron consists of a glomerulus (network of capillaries) and a tubule (proximal end forms a glomerular capsule)
o Renal corpuscle: capsule and glomerulus; site of transfer between blood and nephron
o Filtration barrier: formed of fenestrated endothelium, basal lamina and slit membrane
o Proximal convoluted tubule: single layer of cuboidal cells with microvilli
o Loop of Henle: descending limb (thin; squamous cells) and ascending limb (thick; cuboidal cells)
o Distal convoluted tubule: cuboidal cells; empties into collecting tubule
o Juxtaglomerular apparatus: distal tubule contacts afferent arteriole; composed of juxtaglomerular cells of afferent arteriole and macula densa of tubule; secretes renin

Special features of blood flow through the kidney
o Two capillary beds: (1) glomerulus and (2) peritubular capillaries
o Afferent and efferent arterioles maintain constant blood pressure in glomerulus

Physiology of the kidneys: renal tubules maintain composition, volume and pH of blood and tissue fluid by means of glomerular filtration, tubular reabsorption and tubular secretion
As homeostatic regulators, kidneys remove more or less water according to water intake and loss. Dissolved substances are categorized as to how much they are maintained in the body fluids:
n high threshold substances: maintained at relatively high levels such as glucose, amino acids, fatty acids, glycerol, vitamins and hormones
n medium threshold substances:mineral ions such as sodium, chlorine, hydrogen and hydroxide ions and other organic substances
n low threshold substances: mostly wastes like urea, medicines e.g. aspirin, antibiotics, etc.
As organs for urine formation, blood enters through the renal artery which branches into the afferent arterioles that conduct blood into the glomeruli and exits through the efferent arterioles. Filtered blood leaves the kidneys through the renal veins.
- Glomerular filtration of water and dissolved substances out of the blood in the glomeruli and into Bowman's capsule;
- Tubular reabsorption of water and dissolved substances out of the kidney tubules back into the blood (note that this process prevents substances needed by the body from being lost in the urine);
- Tubular secretion of hydrogen ions (H+), potassium ions (K+), ammonia (NH3), and certain drugs out of the blood and into the kidney tubules, where they are eventually eliminated in the urine.
for a detailed discussion on urine formation, click here.
2. Ureters
n Urine transport: from renal pelvis to urinary bladder; retroperitoneal; entry into the urinary bladder is guarded by a valve-like narrow region preventing backflow of urine into the kidneys
n Three-layered walls:
Inner mucosal layer: transitional epithelium
Middle muscular layer: peristaltic contractions
Outer fibrous layer
3. Urinary Bladder
n Hollow muscular organ: urine storage; retroperitoneal; lined with transitional epithelium; three layers of smooth muscle
n Micturition (urination)
o full bladder activates spinal reflex that causes muscles of bladder wall to contract, resulting in micturition
o impulses from brain can facilitate or inhibit reflex emptying of bladder; with training, can come under voluntary control
4. Urethra: muscular tube lined with mucous membrane; carries urine from bladder to exterior of body; surrounded by external urethral sphincter where it passes through urogenital diaphragm
n Female: short; runs along anterior surface of vagina
n Male: functions in urine passage and reproduction; long
3 parts:
Prostatic urethra: passes through prostate gland
Membranous urethra: passes through urogenital diaphragm
Penile (=Spongy) urethra: passes through penis
Composition of Urine: approx. 95 per cent water and the following dissolved substances:
Nitrogenous wastes (urea, uric acid, ammonia, creatinine); electrolytes; toxins; pigments; hormones; normal pH is generally slightly acidic with a normal transparent yellow/amber/straw color
Clinical conditions
n Acute renal failure: a sudden loss of kidney function, usually associated with shock or intense renal vasoconstriction, that lasts for a few days to as long as three weeks. In most cases the kidney damage is repairable.
n Azotemia: excessive blood nitrogen compounds
n Blood urea nitrogen (BUN): an index of the accumulation of urea and other nitrogenous wastes in the urine, and thus of renal dysfunction. Normal range: 8 to 25 g/L
n Chronic renal failure: a progressive destruction and shrinking of the kidneys, which become incapable of producing urine. It may be caused by chronic glomerulonephritis or pyelonephritis. Because of the permanent damage, the options for sustaining life are hemodialysis or kidney transplant.
n Cystitis: urinary bladder inflammation that produces frequent, burning urination and blood in urine; more common in women, probably because urethra is short
n Cystoscopy: inspection of the urinary system by means of a cystoscope. Tissue and urine samples are obtained for diagnosis and for detection of obstructions.
n Glomerulonephritis: inflammatory condition that affects glomeruli; due to allergic reaction to toxins produced by streptococci bacterial infection in other body parts. If the infection is not treated, the glomeruli are replaced by fibrous tissue, and chronic renal disease may develop.
n Hematuria: blood in the urine
n Hemodialysis: a technique for purifying the blood outside the body.
n Kidney stones (renal calculi; nephrolithiasis): formed in renal pelvis or urinary bladder by combination of uric acid, calcium oxalate and calcium phosphate; may cause urine retention, pain and infection due to blockage of ureters and ulceration of urinary tract lining.
n Nocturia: night urination during sleep
n Oliguria: a diminished quantity of urine
n Polyuria: excessive urine output
n Pressure-related pathologies:
Prostate hypertrophy: can cause fluid backup that interferes with regulation of body fluid composition
Low arterial blood pressure: reduces ability of kidneys to form glomerular filtrate
n Pyelography: intravenous injection of a radiopaque dye that permits X-ray examination of the kidney, ureters and urinary bladder as the dye pass through the urinary system.
n Pyelonephritis: bacterial infection of renal pelvis and surrounding tissue, which, if not treated, spreads progressively into the calyces and tubules of the nephrons.
n Proteinuria: plasma proteins pass into urine
n Renal clearance: the volume of blood plasma per minute that is cleared of a given substance if
U = concentration of substance in urine, mg/ml
P = concentration of substance in plasma, mg/ml
F = urine flow, ml/min
Then, renal clearance = UF/P
n Uremia: metabolic products, including urea, accumulate in blood due to improper excretion
n Urethritis: inflammation of the urethra
n Urinalysis: measurement of urine volume (750 to 2000 ml/day), pH, specific gravity, protein, mucin, ketone bodies, bilirubin, glucose, blood cells, epithelial cells and casts
Comments (0)
You don't have permission to comment on this page.